Last August, KJ Muldoon was born with a potentially fatal genetic disorder. Just six months later, he received a Crispr treatment designed just for him.
Muldoon has a rare disorder known as CPS1 deficiency, which causes a dangerous amount of ammonia to build up in the blood. About half of babies born with it will die early in life. Current treatment options—a highly restrictive diet and liver transplantation—aren’t ideal. But a team at the Children’s Hospital of Philadelphia and Penn Medicine was able to bypass the standard years-long drug development timeline and use Cripsr to create a personalized medicine for KJ in a matter of months.
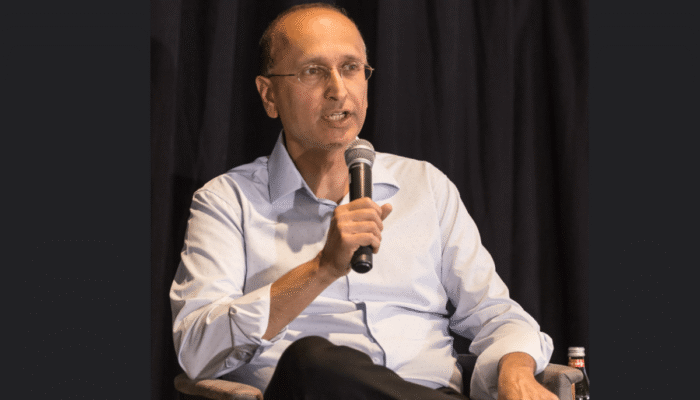
“We had a patient who was facing a very, very devastating outcome,” says Kiran Musunuru, professor for translational research at the University of Pennsylvania and Children’s Hospital of Philadelphia, who was part of the team that made KJ’s treatment.
When KJ was born, his muscles were rigid, he was lethargic, and he wouldn’t eat. After three doses of his custom treatment, KJ is starting to hit developmental milestones his parents never thought they’d see him reach. He’s now able to eat certain foods and sit upright by himself. “He really has made tremendous strides,” his father Kyle Muldoon says.
The case is detailed today in a study published in The New England Journal of Medicine and was presented at the American Society of Gene & Cell Therapy annual meeting in New Orleans. It could provide a blueprint for making customized gene-editing treatments for other patients with rare diseases that have few or no medical treatments available.
When the body digests protein, ammonia is made in the process. An important enzyme called CPS1 helps clear this toxic byproduct, but people with CPS1 deficiency lack this enzyme. Too much ammonia in the system can lead to organ damage, and even brain damage and death.
Since KJ’s birth, he has been on special ammonia-reducing medicines and a low-protein diet. After receiving the bespoke Crispr drug, though, KJ was able to go on a lower dose of the medication and start eating more protein without any serious side effects. He’s still in the hospital, but his doctors hope to send him home in the next month or so.
Both KJ’s parents and his medical team stop short of calling the Crispr therapy a cure, but they say it’s promising to see his improvement. “It’s still very early, so we will need to continue to watch KJ closely to fully understand the full effects of this therapy,” says Rebecca Ahrens-Nicklas, director of the Gene Therapy for Inherited Metabolic Disorders Frontier Program at Children’s Hospital of Philadelphia and an assistant professor of pediatrics at Penn Medicine, who led the effort with Musunuru. She says the Crispr treatment probably turned KJ’s severe deficiency into a milder form of the disease, but he may still need to be on medication in the future.
Ahrens-Nicklas and Musunuru teamed up in 2023 to explore the feasibility of creating customized gene-editing therapies for individual patients. They decided to focus on urea cycle disorders, a group of genetic metabolic conditions that affect the body’s ability to process ammonia that includes CPS1 deficiency. Often, patients require a liver transplant. While the procedure is possible in infants, it’s medically complex. Ahrens-Nicklas and Musunuru saw an opportunity to find another path.
When KJ was born, the researchers used genome sequencing to determine the specific genetic mutation driving his disease. It turns out KJ had actually inherited two different mutations in the CPS1 gene—one from each parent. The team decided to target the mutation that had been reported before in an unrelated patient known to have severe CPS1 deficiency; the other hadn’t been seen before.
KJ’s team turned to Crispr, the Nobel Prize-winning technology that can precisely edit DNA. So far, only one Crispr-based medicine is commercially available. Approved in late 2023, it treats sickle cell disease and beta thalassemia. Other Crispr-based therapies are in development for more common diseases that affect tens or hundreds of thousands of patients.
The allure of Crispr is its potential to directly address the underlying genetic cause of a disease rather than simply treat symptoms, as the vast majority of current medicine does. The approved Crispr therapy, Casgevy, is given as a one-time treatment. But the Philadelphia-led team specifically designed KJ’s therapy to be redosable out of safety concerns, starting with a low dose to ensure there were no adverse effects. Terry Horgan, a 27-year-old with Duchenne muscular dystrophy, passed away in 2022 shortly after receiving the first known custom Crispr treatment. His death was likely due to a reaction to the virus used to deliver the Crispr molecules.
For KJ’s treatment, researchers used a version of Crispr called base editing that can change one “letter” in a DNA sequence to another. They packaged the base-editing components in tiny bubbles called lipid nanoparticles, which were then delivered via an IV infusion.
Before it could be given to KJ though, it was tested for safety in mice and monkeys. Since the drug was unapproved, the team needed permission from the Food and Drug Administration to use the experimental treatment in an individual patient. The researchers applied to the FDA on February 14 and received approval on February 21. They gave KJ his first dose on February 25.
“The clinical responses described are impressive,” says Timothy Yu, a neurologist at Boston Children’s Hospital who wasn’t involved in making KJ’s treatment. He says the Philadelphia team’s approach was a “very thoughtful and comprehensive end-to-end process.”
Yu’s lab has been working on customized genetic medicines based on antisense oligonucleotides, or ASOs—short molecules that block the production of proteins. Yu developed a personalized ASO in 10 months for a young girl with Batten disease, a rare and fatal neurodegenerative disorder. The treatment was dubbed milasen, after the patient, Mila. It was the first medicine that was tailor-made to treat a single patient’s genetic mutation. The treatment temporarily improved Mila’s condition and quality of life, but ultimately, she died in February 2021 at 10 years old.
“The superpower of Crispr base editing is its broad applicability to many types of genetic mutations. Its kryptonite is that we are in the very early days of demonstrating efficient and safe Crispr delivery to many different organs,” Yu says. ASOs, meanwhile, are well vetted for use in the brain, spinal cord, and eye, which are more difficult to address with Crispr.
Crispr could potentially address a variety of genetic diseases and types of cancer, but getting it to the right place in the body remains a challenge. The approved Crispr medicine, Casgevy, involves removing a patient’s cells and editing them outside the body, an arduous and expensive process. A drug given directly to the body would be much more practical. The liver is an easy first target because lipid nanoparticles naturally gravitate there, but only some diseases can be treated in this way.
Since urea cycle disorders primarily originate in the liver, they could be a prime target for custom Crispr medicines. “We’ve just written a new playbook,” says Fyodor Urnov, scientific director at the Innovative Genomics Institute at UC Berkeley, who collaborated on the paper.
Urnov says KJ’s case demonstrates that bespoke genetic treatments can be made quickly and used successfully to treat critically ill patients. “This could have failed in so many ways,” he says. “Nothing was a given.” Every day, he worried that KJ would pass away before they could finish making the therapy.
The team did not say exactly how much the therapy cost to produce, but Musunuru says it was comparable to the cost of a liver transplant, around $800,000. The companies involved in manufacturing—Aldevron, Danaher, and Integrated DNA Technologies—made in-kind contributions.
“Though it will take a lot of work to get there, my hope is that someday no rare disease patients will die prematurely from misspellings in their genes, because we’ll be able to correct them,” Musunuru says.